Unlocking Discoveries Safely: Using the primary care data of 59 million patients to determine the impact of the COVID-19 pandemic on antipsychotic prescribing in at-risk populations
-
Authors:
Millie Green
-
Posted:
- Categories:

In 2021 the OpenSAFELY platform grew and we were able to use patients’ GP records from approximately 96% of the English population for studies into COVID-19. This was only made possible by our team developing innovative new methods to protect privacy, and through using highly secure federated analytics of patient data at source. This momentous development allowed us to begin carrying out a number of federated analyses, the latest of which has just been published in BMJ Mental health. In this study, we explored the prescribing trends of antipsychotics in at-risk patient groups over the course of the COVID-19 pandemic using 59 million patients’ primary care records, and in the following blog Millie Green explains some of our findings.
Federated analytics in OpenSAFELY
Federation allows researchers to write code for data curation and analysis once, and then run it in multiple locations where sensitive patient data is stored. The researchers can then retrieve summary outputs that have been assured not to contain sensitive data, and combine these outputs for further analysis. This means raw clinical data never has to leave its original (and secure) location, even when research spans different databases.
Empowering Research
From the beginning, OpenSAFELY was designed with federation in mind, having been shaped around the principle that very sensitive data should be copied or moved as infrequently as possible. The ability to undertake federated analytics using OpenSAFELY greatly increases the precision (by using 59 million records!), and ensures that the population being studied is representative of the whole population (because it very nearly is the whole population of England). This increases the ability to do groundbreaking work to improve people’s health, as well as the healthcare system. This is all possible without compromising the security and privacy of the sensitive information, and while ensuring ethical and regulatory compliance. The OpenSAFELY approach to federated analytics also maintains public trust, by making all analyses transparent and publicly auditable.
Unlocking Innovation Safely
The ability to undertake a federated analysis using the OpenSAFELY platform was a truly massive technical achievement and speaks to the strength of the OpenSAFELY collaborative; this includes all of the support and generous assistance received from researchers, software developers, the EMIS and TPP Technical Operations teams and the information governance and database teams at NHS England and the NHS England Transformation Directorate. It was driven, as ever, by the combination of skills that no single individual, or even team, is ever likely to embody alone, across EHR data analysis, EHR system design, software development, data management, open science, and more.
Our latest study
Our latest study, published in BMJ Mental health describes how we used the OpenSAFELY platform to explore prescribing trends of antipsychotics in at-risk patient groups over the course of the pandemic. Specifically, we explored the impact of the COVID-19 pandemic on antipsychotic prescribing in patients with autism, dementia, learning disability, serious mental illness or those living in a care home. We believe this is the most granular study to date over such a large population, describing antipsychotic prescribing trends within these vulnerable patients.
What approach did we use?
This analysis was delivered using federated analysis through the OpenSAFELY platform: codelists and code for data management and data analysis were specified once using the OpenSAFELY tools; then transmitted securely to the OpenSAFELY-TPP platform within TPP’s secure environment, and separately to the OpenSAFELY-EMIS platform within EMIS’s secure environment, where they were each executed separately against local patient data; summary results were then reviewed for disclosiveness, released, and combined for the final outputs.
What did we find?
Over the study period, there was a slight increase in the overall rate of antipsychotic prescribing (per 1000 patients) from 8.67 (95% CI 8.66 to 8.68) in January–March 2019 to 9.09 (95% CI 9.07 to 9.10) in October–December 2022 (Figure 1). When broken down by at-risk populations, we observed a gradual increase in antipsychotic prescribing in patients with dementia and in those residing in care homes, and a gradual decrease in antipsychotic use in patients with learning disability or autism over the study period.
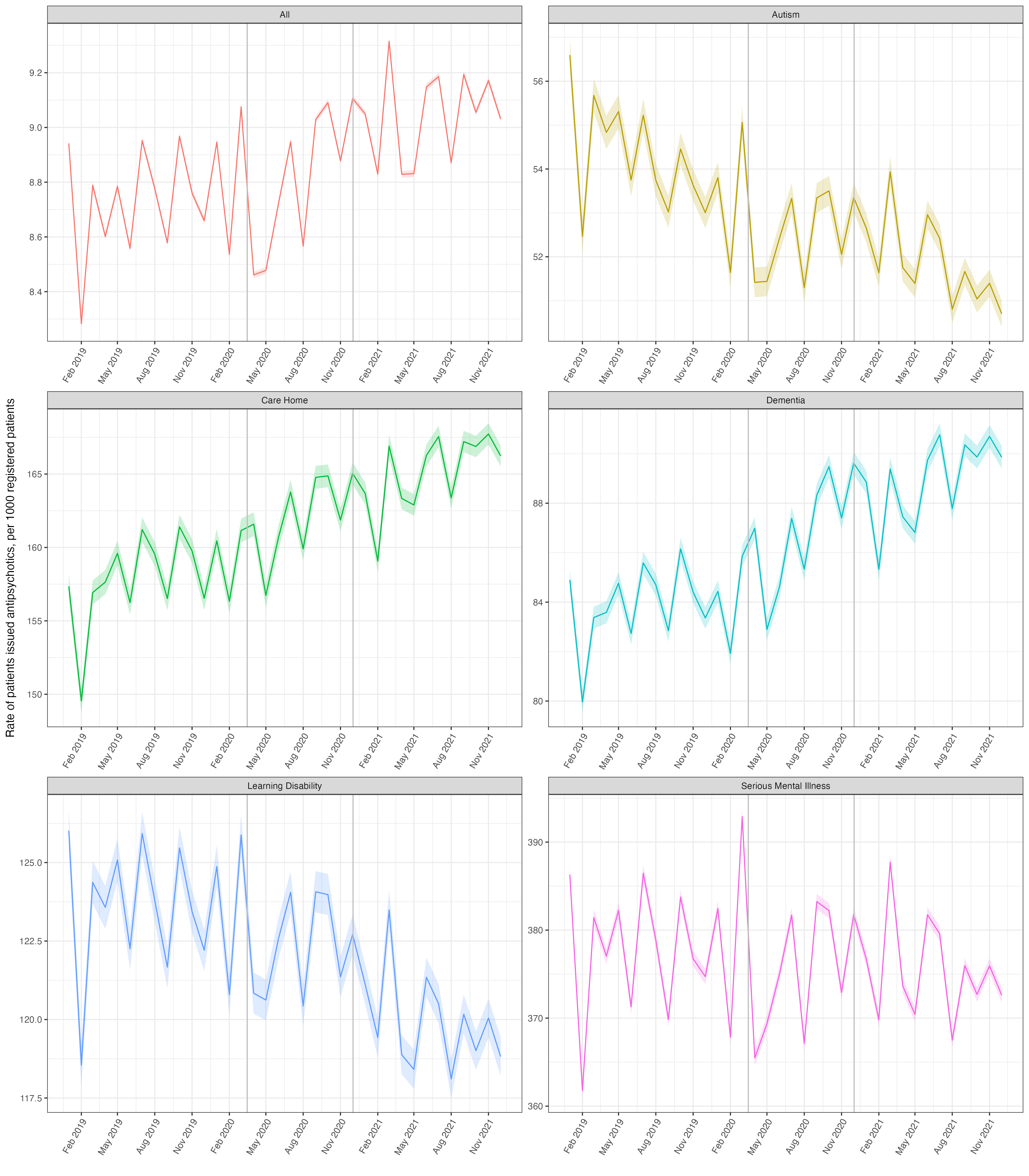 Figure 1 Monthly rate of patients issued an antipsychotic between January 2019 and December 2021, stratified by at-risk group. Solid coloured lines represent the monthly rates for each group with shaded colours areas representing 95% CIs. Vertical grey lines represent the start of the first two national lockdowns. Note each plot has a separate y-axis scale thus plots should be considered separately.
Figure 1 Monthly rate of patients issued an antipsychotic between January 2019 and December 2021, stratified by at-risk group. Solid coloured lines represent the monthly rates for each group with shaded colours areas representing 95% CIs. Vertical grey lines represent the start of the first two national lockdowns. Note each plot has a separate y-axis scale thus plots should be considered separately.
There was a decrease in the overall rate of new initiation of antipsychotics around the time of the first lockdown; in Quarter 2 of 2020 this figure was 0.794 (95% CI 0.791 to 0.799) whereas in Q2 2019 it was 0.895 (95% CI 0.891 to 0.899) (Figure 2). When broken down by at-risk populations, we observed a spike in antipsychotic prescribing in the dementia and care home groups which coincided with the beginning of the first and second lockdowns, with results from our sensitivity analysis supporting the hypothesis that these spikes were due to palliative care prescribing.
We also observed a decreasing trend in the prescribing of antipsychotics in patients with learning disability or autism, although we found some notable variations in frequency of use associated with ethnicity which requires further investigation. We did not observe an increase in new prescriptions for antipsychotics in the learning disability and autistic population and found no consistent changes in the prescribing trends of antipsychotics in patients with a severe mental illness.
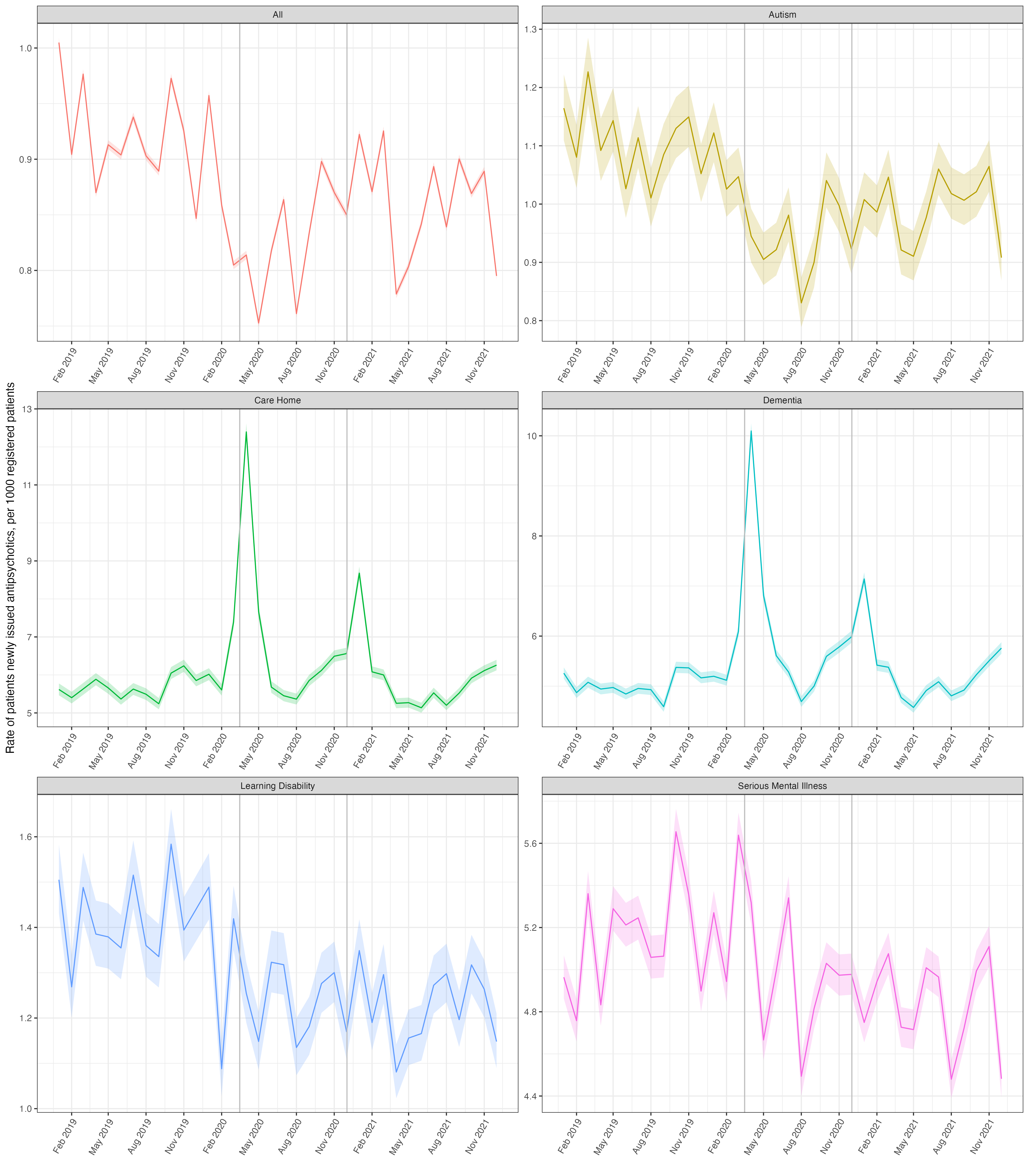 Figure 2 Monthly rate of patients newly issued an antipsychotic between January 2019 and December 2021 stratified by at-risk group. Solid coloured lines represent the monthly rates for each group with shaded colours areas representing 95% CIs. Vertical grey lines represent the start of the first two national lockdowns. Note variation in each plot has a separate y-axis scale thus plots should be considered separately.
Figure 2 Monthly rate of patients newly issued an antipsychotic between January 2019 and December 2021 stratified by at-risk group. Solid coloured lines represent the monthly rates for each group with shaded colours areas representing 95% CIs. Vertical grey lines represent the start of the first two national lockdowns. Note variation in each plot has a separate y-axis scale thus plots should be considered separately.
Summary
Our study shows that over the course of the pandemic there were increases in antipsychotic use in certain at-risk populations, specifically patients with dementia and those who reside in care homes. There were brief increases in antipsychotic prescribing in patients with dementia or in those who were resident in care homes during each of the lockdown periods which are likely to be due to palliative care prescribing. We also found there was a decrease in antipsychotic prescribing in patients with learning disability or autism.
While these results provide some insights into the prescribing trends of antipsychotics in at-risk patient groups over the course of the COVID-19 pandemic, there is still much to learn about how the pandemic and subsequent lockdowns have affected the mental health of at-risk populations. There is a need to continue to promote and support research and policy development that reduce inappropriate prescribing of antipsychotics within these vulnerable groups of patients.
For detailed results and in depth discussions, read the full paper.
Get in touch!
If you, or a group you know of, are interested in our study or with working on federated analytics, we’d love to hear from you at team@opensafely.org.

