Trends in inequalities in avoidable hospitalisations across the COVID-19 pandemic
-
Authors:
Mark Green
-
Posted:
- Categories:

This article is part of a series: Guest blogs
- Conducting Research Using OpenSAFELY: My Experience of the Co-pilot Service
- High Dose Dexamethasone
- How I use OpenPrescribing in my practice as a GP
- Conducting Research Using OpenSAFELY: My Experience of the Co-pilot Service
- Using electronic health records and open science in the COVID-19 pandemic
- Exploring the Impact of COVID-19 on common infections: Treatment Pathways, Antibiotic Prescribing, and Exposure
- Incidence and management of inflammatory arthritis in England before and during the COVID-19 pandemic
- Updates of OpenSAFELY Research on COVID-19 Therapeutics
- Understanding Repeat Antibiotic Prescribing in the Pandemic: Insights On Health Inequalities
- Trends in inequalities in avoidable hospitalisations across the COVID-19 pandemic
In this guest blog, Mark Green describes their latest paper using OpenSAFELY.
Background
There has been public, political and media concern that the disruption in accessing healthcare during the COVID-19 pandemic would increase hospital admissions due to people not receiving necessary care. Answering whether this was the case is difficult. The journey from onset of illness to accessing care is complex, making attributing specific events of disruption (if even measurable) to outcomes practically impossible.
In our newly published paper, we used ‘avoidable hospital admissions’ as a proxy for investigating the impacts of healthcare disruption. Avoidable hospitalisations are emergency (unplanned) hospital admissions that could potentially have been prevented if individuals had received timely care within the community (and therefore may be susceptible to disruptions to care). Through exploring trends in avoidable hospital admissions in OpenSAFELY during the COVID-19 pandemic, we can see if periods of disrupted access (e.g., lockdowns) resulted in more avoidable hospital admissions.
Changing trends in avoidable admissions
We found that across numerous measures of avoidable hospital admissions significantly fell during the first national lockdown in 2020 (Figure 1). While rates increased following the end of the lockdown, they did not increase to the same levels as observed in 2019. Subsequent falls were observed in other lockdowns, but never to the same extent as in the first lockdown. The exception to this was for vaccine-preventable ambulatory conditions which remained significantly lower throughout the whole study period, partly due to the low rates of influenza circulating over the study period.
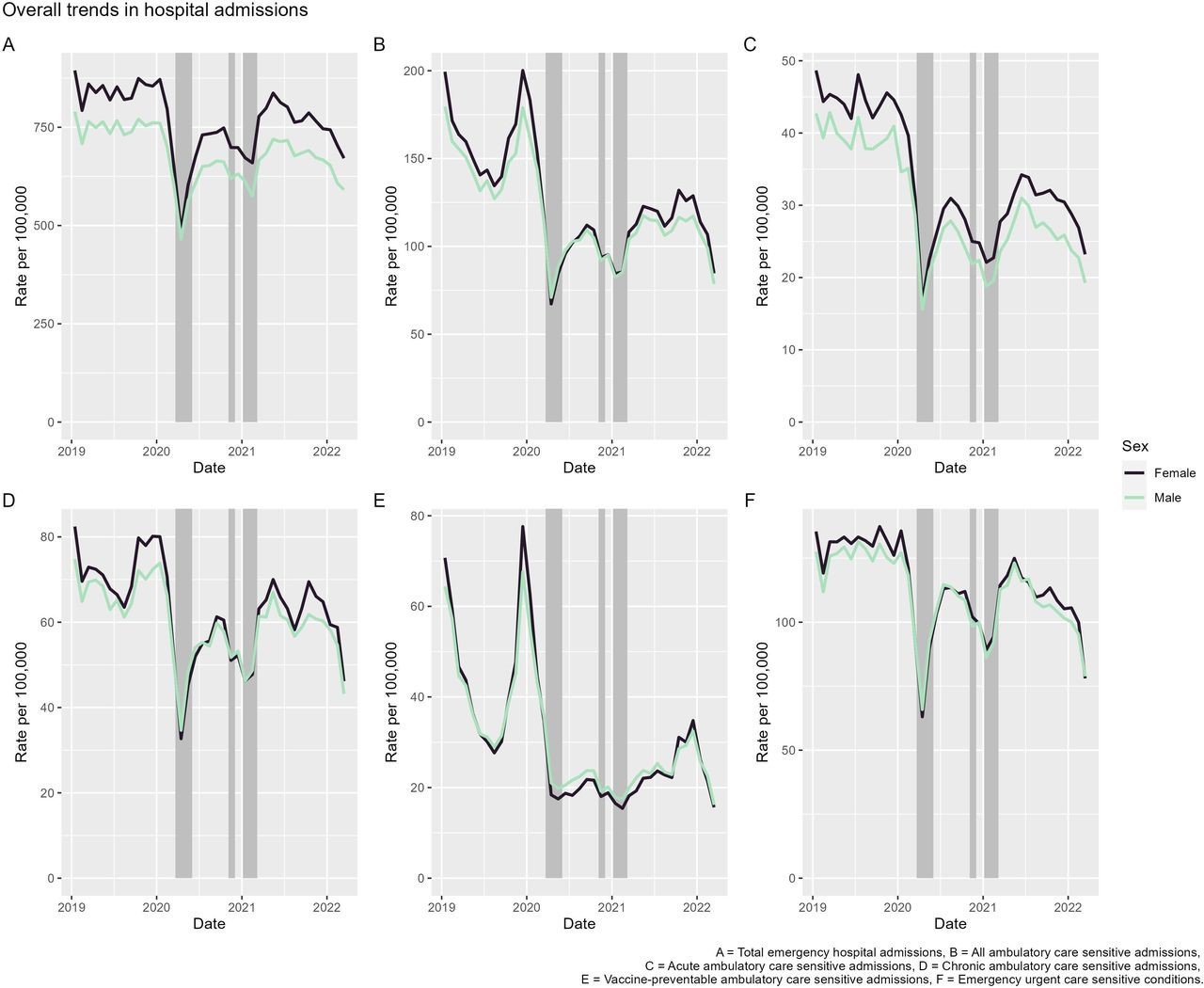 Figure 1: Crude hospital admission rates (per 100 000 population) by sex for measures of avoidable hospitalisations. Shaded periods represent national lockdowns.
Figure 1: Crude hospital admission rates (per 100 000 population) by sex for measures of avoidable hospitalisations. Shaded periods represent national lockdowns.
While one interpretation might therefore be that the impacts of healthcare disruption were minimal, we should not forget that healthcare disruption is part of the explanation for the trends we observe. The extent of declines in trends is likely to reflect significant changes in patient behaviour (e.g., fear of being exposed to SARS-CoV-2 in healthcare settings, not wanting to burden services in a crisis) and access to health systems (e.g., physicians deciding not to refer patients to hospital, changes in how admissions are made, prioritisation of community care).
Narrowing social and spatial inequalities
The impacts of the COVID-19 pandemic have in many respects been highly unequal. Our results showed evidence on the unequal distribution in avoidable hospital admissions across social and spatial markers of inequality (ethnic group, socioeconomic deprivation and geographical region). However, when we estimated how the level of inequality changed from the COVID-19 pandemic onwards we found that for these three measures that inequalities narrowed. The narrowing of inequalities was greatest during the first national lockdown. Following this period, levels of inequalities remained lower than in 2019.
This was contrary to our predictions given the widening of inequalities reported elsewhere for other health outcomes. It suggests that the changing trends in inequalities are not always so obvious, consistent and often nuanced in their interpretation. Although inequalities narrowed, there were still differences between regions, ethnic groups and levels of deprivation reminding us that inequalities remain important.
Why this matters
The COVID-19 pandemic has affected avoidable hospitalisations in unexpected and potentially surprising ways. It provides some reassurance over the resilience of our health system in absorbing external shocks, as well as the hard work in reorganising care to support responses to COVID-19. Only through using OpenSAFELY could we track these impacts in real-time and respond to their emerging trends.
Get in touch
All of the code used for the paper is openly available here.
You can read the full paper at: Green MA, McKee M, Massey J, et al. Trends in inequalities in avoidable hospitalisations across the COVID-19 pandemic: a cohort study of 23.5 million people in England. BMJ Open 2024;14:e077948

